Drug Box Awesomeness
 The greatest call of the day/week/month came out as chest pain. We arrived to find our patient who only spoke Spanish with no translator in sight. Oh yeah, what made it a pretty hilarious call as well was the fact that I had a paramedic student with me.
The greatest call of the day/week/month came out as chest pain. We arrived to find our patient who only spoke Spanish with no translator in sight. Oh yeah, what made it a pretty hilarious call as well was the fact that I had a paramedic student with me. So, the student started to attempt doing his thing, although none of us spoke comprehensible Spanish, while the firefighters went to get the stair chair. When they returned, one of them for some reason inquired “Why is she on a nasal cannula?”
Although I’m sure that some of my colleagues would point to the paramedic patch on their left shoulder and say “That’s why!”
I, however merely attempted to explain that I believe a nasal cannula has more uses than for tying things together. Where a mask can feel constricting, a nasal cannula can deliver oxygen without raising the anxiety of the patient, the patient can still get a relatively high concentration of oxygen, and although you think she appears to be ‘gasping for breath,’ I think she is doing alright, also her pulse ox is 99% and why am I still explaining this to you? We need to get out of here.
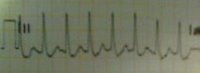
After stairing her down three flights of ridiculously steep stairs, we got her safely outside and in the ambo. Vitals, monitor, IV. I follow my partners gaze to the screen of the lifepack 12 to discover SVT, which is basically when you’re heart is beating uncontrollably and abnormally fast. She was going at a rate of 186 at one point, about three times faster than my resting heart rate.
Luckily, an English and Spanish speaking neighbor materialized out of nowhere and knocked on the ambo doors. She didn’t mind translating for a minute for us. The student, bless him, tried to explain vagal maneuvers to the translator, which I think the patient understood, but they did not help her. (If you stimulate a particular cranial nerve, sometimes tachycardia can be ‘broken,’ this is what we were attempting)
When that didn’t work and the translator unfortunately left, I decided to break out the adenosine. This is a drug best described as a chemical defibrillator. It essentially can stop the heart, and cause it to (ideally) reset to a more normal rhythm. I had never pushed it before, so I was a little nervous, plus it was difficult to explain to the patient that she was about to feel more than a little weird. (‘Muy mal’ was all I could come up with, but she already felt bad.)
So I drew it up and handed it to the student who, I later learned, couldn’t believe we were carrying out a textbook case like this. I prepped a flush, and we pushed. It’s an exciting drug because you have to push it really fast and then flush it immediately so that it goes through the blood stream very quickly. Then we all stopped and waited. Seconds ticked by, then suddenly, just as we had almost given up, the heart rate went from 180s, 160s, 120s and then ended up hovering around 110. I could barely contain my excitement. “Esta bien?” I asked, and she shook her head yes, looking relieved and quite a lot better.
Now, I love all the drugs in the drug box, but it seems that every time I use a new one, it becomes the reigning favorite. Although we didn’t get the characteristic period of asystole that can sometimes happen with the drug, it was still amazing.
Every once in a while this paramedic thing really comes in handy.


Comments
Sounds like a good call. Nice job, paramedic! (And thanks for your nice comment on my blog.)